In 1891, almost 20,000 Egyptians died in Cairo. This was a relatively average year. There was no particular pestilence; the plague had been gradually receding from the city since the 1840s, and most of the dead had succumbed to the usual illnesses and conditions of the 19th century: Dysentery, typhoid, tuberculosis, childbirth and old age had claimed the majority of victims. But just 19 died from cancer. This was also nothing unusual. From 1889 to 1891, of the nearly 13,000 patients at the Kasr-el-Aini Hospital, just 77, a mere 0.6%, received a cancer diagnosis.
Since 1805, Egypt had been ruled by the “Wali” (viceroy) Muhammad Ali and his descendants. The patriarch had been sent by the sultan of the Ottoman Empire in Istanbul to recover the country from Napoleon’s occupation. Ali was an ambitious, reforming leader. He established a dynasty that was to rule Egypt until the revolution of 1952. His primary focus was the military, but he also attempted to modernize the country. He sent students to Europe and invited training missions to Egypt. He reformed the civil service and built a system of canals for irrigation and transport. Over the ensuing decades, Egyptian trade flourished, and merchants and their ships became increasingly crucial to the country’s economic success. But as with so many places around the world, success and reform did little to prevent British busybodies from meddling in Egyptian affairs. In 1882, this meddling turned into indirect rule, when Egypt became a British protectorate.
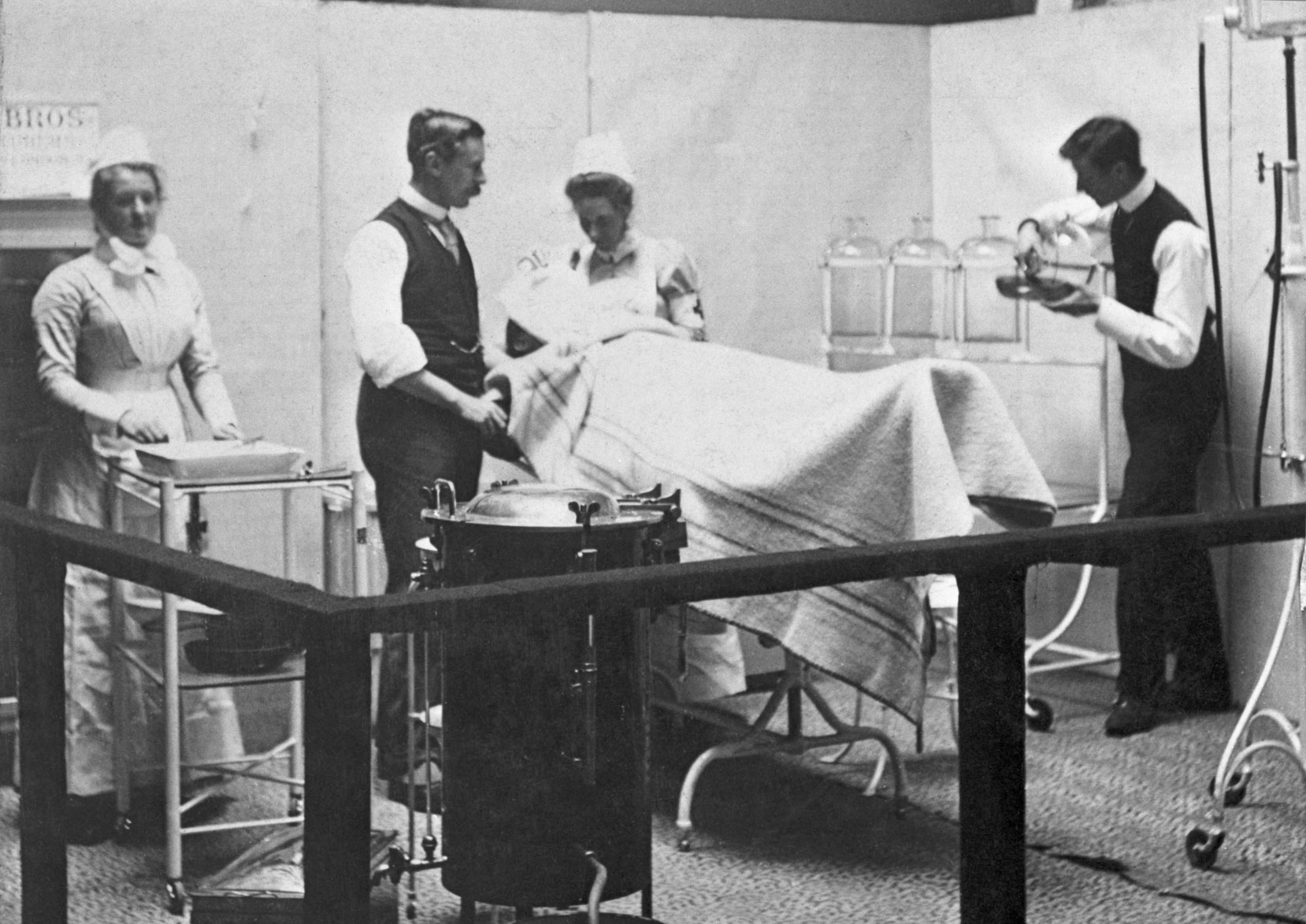
Medicine was a key part of Britain’s imperial arsenal. Colonial doctors, sent far and wide, were the empire’s eyes and ears. They not only reported back on the health conditions of Indigenous populations but also surveyed behaviors and used epidemic disease as excuses to impose restrictions on civil liberties and freedom of movement. Colonized people were research subjects as much as they were patients — the British Empire did not just export customs, political systems and language but imposed a medical structure that suppressed local health knowledge and practices.
Cairo, the capital, had been founded almost a thousand years before the British arrived in Egypt. By the 19th century, however, it was a divided city. “European Cairo” impressed itself upon a pair of visitors in 1909, Augustus Lamplough and R. Francis, “as an English town in which any quantity of novel oriental sights are kept for the aesthetic satisfaction of the inhabitants, much as the proprietor of a country place keeps a game preserve or deer park for his own amusement.” But “Egyptian Cairo” was “practically what it always was.”
The reason Cairo’s cancer rates were remarked upon, and the reason we still have the data in hand today, is that late-Victorian doctors working far from home had started to notice a pattern. In the many and various places Britain had colonized over the course of the 19th century and before, the doctors who had been dispatched from the metropolis to study and treat the sick observed strikingly low rates of cancer among the Indigenous population.
This might not seem that surprising, since the 19th century is supposed to have been an era of epidemic disease. It was a century of high infant mortality, sweeping infections, and deadly bouts of cholera and consumption. By contrast, today we tend to think of cancer as something tied to the 20th century. It was only then that we entered the “cancer age” and only then that we, with our DDT, mass-produced meat and industrial pollution, made the world carcinogenic. And it was only in the late part of that century that U.S. President Richard Nixon proclaimed a “war on cancer.” Malignancy seems to be, as the American physician, biologist and author Siddhartha Mukherjee writes, “the quintessential product of modernity.”
As a result, we know relatively little about cancer before the 20th century. Most historians, even historians of medicine, simply haven’t looked for the disease in their sources and records. But cancer in 19th-century Britain was not only much more common than we now might assume, it also preoccupied the minds, energies and activities of Victorian doctors in remarkable and enduring ways.
In 1899, the English doctor and writer Woods Hutchinson turned his pen to what he called the “Cancer Problem” and, in a metaphorically rich essay, set out a series of anxieties about medical failure, professional identity and the fundamental fragility of the human body. He argued that while Britain might have reined in the powers of epidemic diseases like typhoid and cholera, cancer remained a “riddle of the sphinx.” Despite multiple medical successes — pain-free surgery, sewage systems and bacteriology — 19th-century doctors and scientists had failed in one of their key aims: to understand and effectively treat malignancy. In 1899, cancer remained the “dread disease” and the “emperor of all maladies.”
Hutchinson even made the troubling suggestion that this mysterious disease seemed to be taking advantage of medicine’s ignorance, increasing in incidence and capacity to kill. A few years earlier, the popular newspaper the Pall Mall Gazette reported, “Cancer … stands almost alone as a disease which increases with our prosperity, and while our health laws are raising the standard of public health, the mortality from cancer stands forth as a blot upon the results.” Hutchinson and his contemporaries thought that the number of people dying from cancer in Britain was rising at an alarming rate.
Things were markedly different in the colonies. As one doctor remarked, cancer “prevails extensively in some parts of the globe and is scarcely known in others.” Cancer in British Central Africa, for example, was “of the utmost rarity,” and in Sierra Leone, “cancer as a disease is very rare among the aborigines.” Similar situations were reported from New Guinea (now Papua New Guinea), Ceylon (present-day Sri Lanka), and Hong Kong. These observations were concerning. While cancer might be increasing, the epidemic seemed to be confined to nations that were conventionally understood as culturally, even biologically, superior. This was even true within Europe, where the disease appeared to be more common in wealthier, more “civilized” places like England and Bavaria than in poorer nations like Italy and Ireland.
Civilization was a central preoccupation for Victorians. They wrote about it, worried about it and attempted to subject it to scientific study. It was tied to the notion of degeneracy, an idea that suffused late 19th-century culture and the debates of European and American elites. Fundamentally, it was the idea that prosperity, industrialization and urbanization brought with them a plethora of physical and emotional complaints. And by implication, it guaranteed neither the “natural” triumph of the “civilizing” imperial Western powers nor the stability of the racial order.
A body of literature on degeneration flourished around the turn of the century. These texts dealt with the “apparent paradox” that civilization itself might be the catalyst of, as much as the defense against, physical and social pathology. Now that the West had reached its peak, both bodies and societies were set on a steady path of decline. This was the thinking that underpinned eugenics and its attempts to reverse degeneration and preserve the “quality” elements of Western society.
Ideas about cancer and its global distribution were profoundly influenced by such thinking. If the British Empire was anything like the Roman one, perhaps the end of the 19th century was witnessing a similar collapse. “Anglo-Saxon” and “Teutonic” races had reached their pinnacle and were now suffering increasingly from chronic disease, poor mental health and moral deviancy as a result.
Paradoxically, therefore, 19th-century doctors explained the difference in cancer incidence between England and Egypt by saying that the former was simply more advanced. For some, this was a problem and product of biology — a kind of racial determinism. The idea that certain races were more or less vulnerable to certain diseases was common. In 1883, the erratic and eccentric scientist Charles Creighton wrote that smallpox was “peculiarly an African disease.”
But for most people, cancer was less a product of the civilized body, and more the result of a civilized way of life. Doctors argued that the increasing incidence of the disease in so-called advanced nations occurred because their societies had departed from nature. In particular, they focused on changing diets. Some were concerned that excessive consumption of salt was cancer-causing; others placed the blame with drinking tea, especially in British colonies like New Zealand. There was also a popular strand of thought that located the cause of cancer, and its increase, in the consumption of meat, and various doctors, food scientists and social commentators (including the founder of the popular cereal brand, John Harvey Kellogg) advocated vegetarianism as a preventative measure against malignancy. Of the many thousands of “flesh-abstainers” whom Kellogg had met, he came across only four cases of cancer. “Uncivilized” people were less vulnerable to malignancy because they lived in harmony with the natural world and pursued simple, abstemious habits. They tended to avoid decadent or artificial food and so avoided cancer.
In 1902, London-based surgeon W. Roger Williams attempted to explain the low rates of cancer in Egypt by insisting that their “conditions of existence” were “unfavorable to the development of cancer.” These conditions included “extreme frugality in living; open-air existence, and last — but not least — an alimentation which includes but little animal food.” Doctors could tell that the low incidence of cancer in “uncivilized” places had nothing to do with race or inherent biology because when people moved from place to place or acquired more civilized habits, their cancer rates increased. Dr. Sir William MacGregor described the case of a man indigenous to British New Guinea who developed cancer in his leg after living “practically a European life” for almost eight years. In a particularly unsettling article, one British surgeon described how cancer had been uncommon among enslaved people in the United States because of their “hard work and frugal diet.” Since abolition, Black people had become “almost as prone to cancer as their white neighbors.”
Compared with today, doctors in the 19th century had vastly different ideas about bodies and diseases. Many of their notions about cancer no longer hold up to scientific scrutiny. They were reliant on systems of thought that have since been discredited. That Victorian scientists and medical practitioners were guided by racist and colonialist thinking is troubling but not that surprising. And yet, for all their claims to modernity, objectivity and moral neutrality, medicine and public health continue to be influenced by the ideas of the 19th century.
Take, for example, Dr. Loren Cordain, who describes himself as the “world’s foremost authority on the evolutionary basis of diet and disease” and as “one of the world’s leading experts on the natural human diet of our Stone Age ancestors.” He is the self-proclaimed founder and a champion of the Paleo Diet, which mimics the diet of our hunter-gatherer ancestors. Hugely popular, it is part of the current fad of “clean” eating and has some crossover with the more recent obsession with “keto.”
In 2014, Cordain published an article on his website, “Breast Cancer and Other Cancers: Diseases of Western Civilization.” In it, he claims that cancer was “rare or non-existent in historically studied hunter gatherers and other less westernized peoples.” He quotes various historical authorities, including the Nobel prize-winning physician Dr. Albert Schweitzer, who wrote on his arrival in Gabon in 1913, “I was astonished to encounter no case of cancer.”
Cordain isn’t exactly part of the medical mainstream, but the ideas he promotes have wide cultural currency. It is a well-known and often rehashed trope that cancer constitutes a “pathology of progress” — an unintended consequence of modernity. Or, as the historian of medicine Charles E. Rosenberg puts it, “The notion that the incidence of much late-20th-century chronic disease reflects a poor fit between modern styles of life and humankind’s genetic heritage.” This idea is a direct descendent of Victorian debates. In attempting to explain the differences in cancer incidence between “civilized” and “uncivilized” places, they constructed cancer as a disease of modern life.
But these ideas matter for more than just accurate history writing. Not only do they equip modern-day quacks and charlatans with “evidence” to sell worried consumers alternative diets and lifestyles, supposedly based on a simpler, less carcinogenic time, but they also imply that cancer and other chronic diseases predominantly affect white, wealthy people in the Global North.
This has had a lasting effect on the global and local distribution of cancer resources. Although most women who now die from breast and cervical cancer (for example) live in low- and middle-income settings, global health has neglected the disease, meaning that many people living with cancer in these places go without adequate treatment. Medical and health care funding in and for the Global South prioritizes treatment and containment of infectious diseases rather than chronic conditions like cancer. Even within high-income countries like the United States, there are massive disparities in cancer prevention and care along class, wealth and ethnicity lines. Race still matters for cancer, just not the way Victorians thought.